A team at Northwell Health’s Feinstein Institutes for Medical Research in Manhasset has developed a deep-learning predictive tool to identify which patients do not need to be woken up overnight – allowing them to rest, recover and discharge faster.
The study’s results, based on 24.3 million vital sign measurements, were published in the Nov. 13 edition of Nature Partner Journals Digital Medicine.
Led by Theodoros Zanos, head of the institute’s Neural and Data Science Lab and an assistant professor at its Institute of Bioelectronic Medicine, and in close collaboration with nephrologist Dr. Jamie Hirsch, the team collected and analyzed data from multiple Northwell Health hospitals between 2012 and 2019, which consisted of 2.13 million patient visits.
The team then used a vast body of clinical data from the patient visits, with factors including respiratory rate, heart rate, systolic blood pressure, body temperature, and patient age, to develop an algorithm that predicts a hospitalized patient’s overnight stability, and if they could be left uninterrupted overnight to sleep.
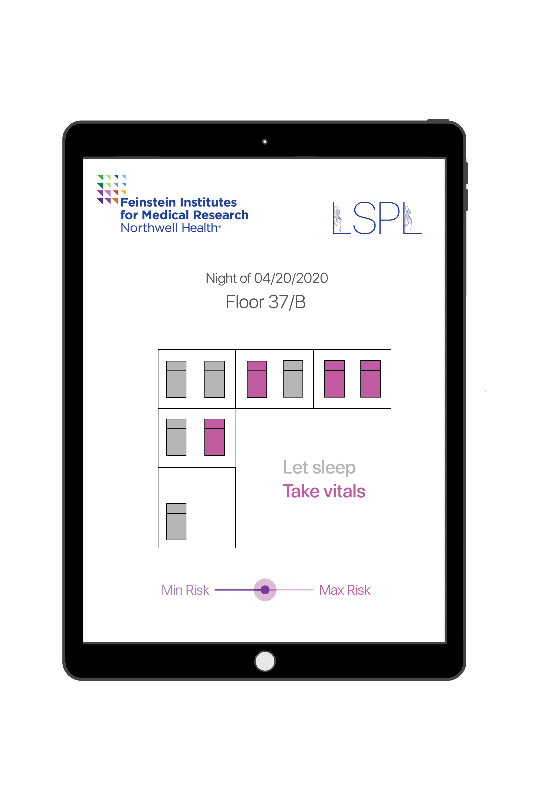
The clinical tool, called “Let Sleeping Patients Lie,” is currently in the process of being rolled out through several hospitals across the Northwell Health system.
“Rest is a critical element to a patient’s care, and it has been well-documented that disrupted sleep is a common complaint that could delay discharge and recovery,” Zanos said. “Our findings highlight the safety and accuracy of machine learning-based solutions to pave the way for more peaceful and safe sleep in a hospital.”
On average, a patient is woken up every four to five hours for vital sign checks. The study revealed that the predictive model salvaged approximately half of the patient’s overnights in a hospital.
The model’s success was achieved with extremely low risk; having only misclassified less than two out of 10,000 patient-nights. The tool also allows clinical teams to adjust the model’s predictive thresholds to implement a more strict patient assessment.
Additionally, to ensure proper care, simple visual inspection of the sleeping patients during typical nurse rounds should suffice in detecting these misclassified patients, a procedure that is already part of standard nursing guidelines.
The potential for implementing the “Let Sleeping Patients Lie” predictive model goes beyond patient care and has the potential to ease the nightly workload of hospital staff, time management, and may help reduce employee stress and burnout.
Nurses spend between 20-35 percent of their time documenting VS, and approximately 10 percent of their shift collecting them. This clinical tool would enable nurses safely and confidently to forgo half of the overnight VS measurements and could result in up to 20-25 percent of workload reduction in a single overnight shift, facilitating focus on more acutely ill patients.
“Dr. Zanos and his team’s expertise in machine-learning enabled them to invent an effective solution for improving sleep,” said Dr. Kevin J. Tracey, president and CEO of the Feinstein Institutes. “Illness and hospitalization impair sleep cycles, and the promise for artificial intelligence in this domain holds significant promise.”
The Neural and Data Science Lab, which Zanos heads, aims to develop the algorithms that will power the next generation of bioelectronic medicine devices to enable early diagnosis, assess disease severity and personalize and adapt therapies. Current projects in the lab include decoding immune and metabolic states from vagal signals, closed-loop optimization of bioelectronic therapies, non-invasive bioelectronic analytics, and clinical predictive models and machine learning applied in healthcare data.
Most recently, Zanos published a paper in the Springer Nature journal, Bioelectronic Medicine, which reported how AI and machine learning tools could be used to aid in making coronavirus disease 2019 clinical decision making.